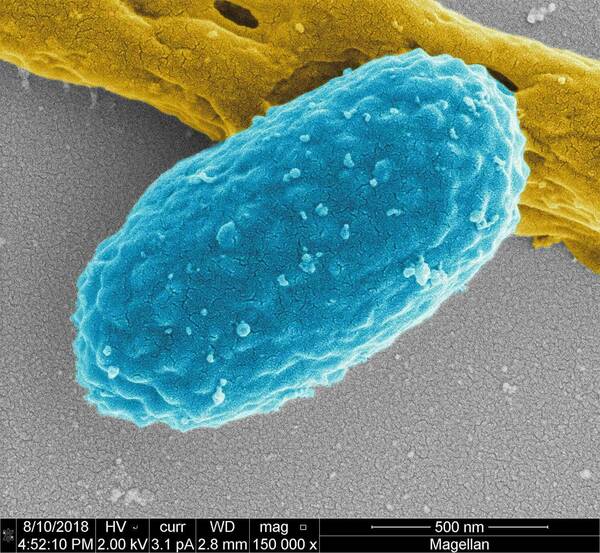
Anyone who has taken antibiotics, and especially those who have recently been in a hospital, nursing home, or other long-term facility, is at risk for developing a potentially life-threatening infection from Clostridioides difficile (C. diff) bacteria—an infection that is notoriously difficult to cure.
But University of Notre Dame researchers realized that an oxadiazole antibiotic—a compound of a previously discovered class that treats MRSA—kills C. diff. and prevents the germination of its spores. The research by Mayland Chang, research professor, and Shahriar Mobashery, the Navari Professor of Life Sciences, both in the Department of Chemistry and Biochemistry, and collaborators was published in the Proceedings of the National Academy of Sciences.

“C. diff spores are the underlying cause of current reinfection,” said Mobashery, adding that bacteria that produce spores are among the most dangerous on earth—anthrax is such a bacterium, for instance. “This recurrence of infection is the cause of significant mortality and morbidity, so to break the cycle of recurrence it’s critical to prevent spores from germinating.”
Their research showed that the new dual-action antibiotic did break the cycle of reinfection. Chang and Mobashery, who are affiliated with the Warren Center for Drug Discovery, described the oxadiazole, which inhibits spore germination, as unlike the approved clinically used antibiotics for C. diff. The most commonly used medication, vancomycin, which does not inhibit spore germination. The oxadiazole, however, breaks down the proteins of the bacterium’s germ cell wall and inhibits another protein that allows for germination.
C. diff’s spores germinate in the small intestine, then travel to the large intestine where they release toxins that can damage tissues while causing extreme diarrhea and other symptoms. Healthy people can tolerate C. diff most of the time, but the spores from C. diff thrive after rounds of antibiotics have killed “healthy” bacteria that keeps the gut functioning well.
Vancomycin has been approved to treat C. diff because it has what is known as low oral bioavailability—meaning it is not efficiently absorbed into the bloodstream. This allows the antibiotic to “sit” in the gastrointestinal tract and usher the spores out of the body through waste. Unfortunately, vancomycin does not work well enough.
When working through possible uses for the oxadiazole as an antibiotic, Chang noticed it had extremely low oral bioavailability. At first the percentage—just 4 % absorption—appeared to be a mistake, but a recheck of the data confirmed the accuracy.
The researchers determined that this low absorption rate could be particularly effective for C. diff.
“So we decided to see if the oxadiazole was active against it, and it turned out that it worked,” Chang said.
The discovery holds the promise of addressing unmet medical needs, Mobashery said.
“It’s exciting because this opens new doors, as we have not done work on C. diff before,” Chang added.
The team has plans to continue investigating the new antibiotic in further studies. In addition to Chang and Mobashery, other researchers on the paper include first author Jeshina Janardhanan, Choon Kim, Yuanyuan Qian, Jingdong Yang, Jayda Meisel, Derong Ding, Enrico Speri, Valerie A. Schroder, William R. Wolter, and Allen G. Oliver, all of Notre Dame.
The work was supported by the National Institute of Allergy and Infectious Diseases, the Eck Institute of Global Health, and the National Institute of General Medical Sciences. Tufts University School of Medicine, BEI Resources, the Cleveland Veterans Affairs Medical Center, Case Western Reserve University, and the R.M. Alden Research Laboratory. The work was also partially supported by the University of Notre Dame Integrated Imaging Facility.
Originally published by at science.nd.edu on May 10, 2023.